Treatment for Your Child’s Hypoplastic Ventricle: Stage II (Glenn)
In hypoplastic left heart syndrome (HLHS), the left side of the heart can't pump blood to the rest of the body. The right ventricle pumps the blood into the pulmonary artery. Blood reaches the aorta through a patent ductus arteriosus, patent foramen ovale, or an atrial septal defect. A connection between the right and left side of the heart is key for survival.
Your child has a heart problem that includes a hypoplastic ventricle. This means that 1 of the ventricles is either too small or is not there. The most common treatment for this problem is heart surgery. This is often done in 3 stages. This sheet explains what is done during the second stage (stage II), also known as the Glenn procedure. The surgery can't fix your child’s heart problem. But it can help ease your child’s symptoms. It may increase your child’s chances of living a more normal life. The healthcare provider can answer your questions and tell you more as needed.
The goals of heart surgery for a hypoplastic ventricle
-
Stage I. Make the 1 working ventricle the main pumping chamber of the heart, sending blood to both the lungs and the body.
-
Stage II. Decrease the workload of the single ventricle. Reduce the mixing of oxygen-poor and oxygen-rich blood.
-
Stage III. Separate the circulation of blood in the heart. This is so there is very little mixing of oxygen-rich and oxygen-poor blood.
What are the risks?
-
Heart rhythm problem (arrhythmia)
-
Problems in the lungs
-
Infection
-
Bleeding
-
Problems with the nervous system, such as seizures or stroke
-
Abnormal buildup of fluid around the heart or lungs
-
Death
Stage II: The bidirectional Glenn (BDG) procedure
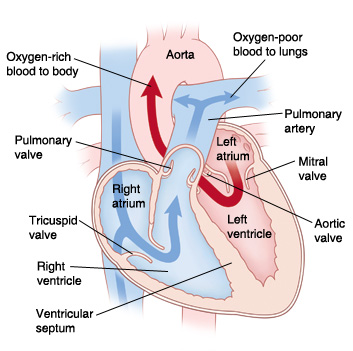 |
| In a normal heart, oxygen-poor blood is pumped to the lungs from the right ventricle. Oxygen-rich blood is pumped to the body from the left ventricle. |
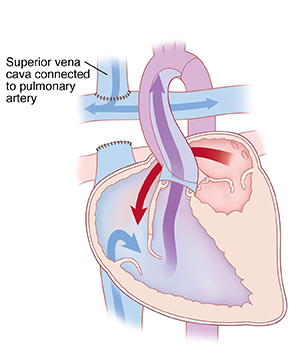 |
| The Bidirectional Glenn procedure sends oxygen-poor blood returning from the upper body directly to the lungs. This helps decrease the workload of the single ventricle. |
The second stage of the surgery is called the BDG procedure. It is most often done when a child is 3 to 6 months old, as your child has outgrown their original shunt and become more cyanotic (skin and lips look blue). Your child may need to stay in the hospital for 5 to 7 days. The procedure gives low-pressure blood flow to the lungs. And it helps reduce the workload of the 1 ventricle. During the surgery, the surgeon:
-
Separates the superior vena cava (SVC) from the heart. The SVC is the large blood vessel that brings oxygen-poor blood from the upper body to the right atrium. This blood vessel is cut from the right atrium. The end closest to the right atrium is closed off. The other end is sewn to the right pulmonary artery. This lets oxygen-poor blood from the upper body flow right to the lungs. It does not pass through the heart. In the lungs, the blood picks up oxygen.
-
Removes any other source of blood flow to the pulmonary artery. If a shunt, band, or other device was placed during a past procedure to direct blood to the lungs, it is removed at this time.
-
Fixes any other areas with problems. For example, a narrowing of the aorta previously repaired in stage I can be fixed.
When to call your child's healthcare provider
Call your child's healthcare provider right away if any of these occur:
-
Redness, draining, swelling, or bleeding at the incision site that gets worse
-
Swelling of the head and neck that gets worse
-
Skin, lips, or nails that look blue (cyanosis)
-
Fever of 100.4°F (38°C) or higher, or as directed by your child's provider
-
Trouble feeding, poor appetite, or poor weight gain
-
Irritability
-
Belly pain
-
Tiredness
-
Cough that won’t go away
-
Nausea or vomiting that continues
-
No clear improvement
When to call 911
Call 911 right away if your child:
Online Medical Reviewer:
Amy Finke RN BSN
Online Medical Reviewer:
Scott Aydin MD
Online Medical Reviewer:
Stacey Wojcik MBA BSN RN
Date Last Reviewed:
8/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.