Exploratory Laparotomy
Exploratory laparotomy is surgery to open up the belly area (abdomen). This surgery is done to find the cause of problems (such as pain or bleeding) that testing could not diagnose. It's also used when an abdominal injury needs emergency medical care. This surgery uses one large cut (incision). The provider can then see and check the organs inside the abdomen. If the cause of the problem is found during the procedure, then treatment is often done at the same time. In some cases, a minimally invasive surgery called exploratory laparoscopy may be used instead. That method uses a tiny camera and several small incisions. But in many cases, an exploratory laparotomy is preferred. Read on to learn more about this procedure.
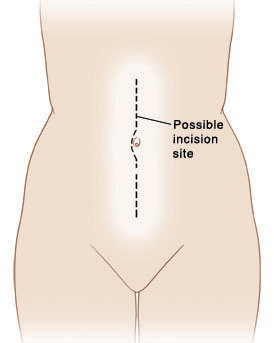 |
| This is an example of the kind of incision the surgeon may use to perform exploratory laparotomy. |
Reasons for the surgery
Organs that may be examined during exploratory laparotomy include:
-
Liver
-
Gallbladder
-
Spleen
-
Pancreas
-
Kidneys
-
Stomach
-
Small intestine (small bowel)
-
Large intestine (colon or large bowel)
-
Appendix
-
Ovaries, fallopian tubes, and uterus (in women)
-
Lymph nodes
-
Abdominal blood vessels
-
Membranes that line the abdominal cavity
Getting ready for the surgery
The surgery takes place in a hospital. It's done by a surgeon. You will likely stay in the hospital for a few days or longer. To get ready for the surgery, do the following:
-
Tell your provider about any medicines you’re taking. This includes over-the-counter medicines, prescription medicines, herbs, illegal drugs, vitamins, and other supplements. You may need to stop taking some or all of them for a time before the surgery.
-
Tell your provider if you drink alcohol. This is very important if you are a heavy drinker. Alcohol withdrawal can be life-threatening. So be honest with your provider.
-
Also tell your provider if you have any allergies or other health problems. This includes recent illnesses, especially any bleeding problems.
-
Stop smoking. Don't smoke on the day of surgery.
-
Follow any directions you are given for not eating or drinking before surgery.
The day of the surgery
-
Many exploratory laparotomy surgical procedures are done on an emergency basis after an injury or accident.
-
You will be checked for risks of heart, lung, or other problems during surgery.
-
You will need to change into a hospital gown.
-
Before the surgery begins, an IV (intravenous) line is put into a vein in your arm or hand. This line supplies fluids and medicines.
-
You will be given medicine (general anesthesia) to keep you free of pain. This medicine puts you in a deep sleep during the surgery.
-
A tube may be placed through your mouth and into your throat to help with breathing during the surgery. Also, monitors are attached to your body. These record your vital signs, such as heart rate, oxygen levels, and blood pressure, during the surgery.
-
A thin tube (catheter) is placed into your bladder. This tube drains urine from your bladder during the surgery. The tube may be left in place after surgery.
During the surgery
-
The skin over your belly is cleaned.
-
An incision is made in your belly.
-
The tissue, blood vessels, and organs in your belly are carefully looked at and checked for problems.
-
Tissue samples (biopsy) may be removed and sent to a lab for study.
-
If the cause of the problem is found, treatment may be done then, if needed.
-
When the surgery is done, the incision is closed with stitches (sutures) or staples. A drain may be placed in the abdomen to remove any extra fluids.
After the surgery
-
You will be taken to the post anesthesia care unit (PACU) to be closely monitored by nurses until you have recovered from the anesthesia. When you are more awake, alert, and stable, you will be moved to your hospital room.
-
Medicines are given to help prevent infection and to manage pain, if needed.
-
You may be able to eat and drink quickly, within 1day of surgery, depending on your situation. You may not be given food or drink until your bowels start to work normally again. This may take a few days.
-
You will need to get up and walk around with help as soon as you are able. This helps to prevent blood clots.
-
You may also be given cough and deep breathing exercises to do. These help prevent pneumonia.
-
The tube to drain urine may be left in place for a few days or removed after surgery.
-
If a drain was used for your incision, this is often removed. before discharge. If not, you will be instructed on how to care for and empty the drain at home.
-
You will be able to go home when the provider says there are no issues of concern.
-
Arrange for an adult family member or friend to drive you home.
-
Before leaving, make sure you have all the prescriptions and home care instructions you will need. Also make sure you have a contact number for your provider or the hospital. This is in case you have problems or questions after the surgery.
-
Prevent constipation, especially if you were prescribed opioid pain medicines. Take fiber as directed and follow bowel care instructions from your provider.
-
Don't lift anything heavier than 5 pounds for about 6 weeks. This gives tissue time to heal, and can prevent a hernia.
When to call your healthcare provider
After you get home, call your healthcare provider if you have:
-
Fever of 100.4°F (38.0°C) or higher, or as advised by your provider
-
Chills
-
Increased pain, redness, swelling, bleeding, or drainage at the incision site
-
Pain that can't be controlled with the medicines prescribed for you
-
Swollen belly
-
Diarrhea or constipation that does not get better in 2 days
-
Bloody or black, tarry stools
-
Problems or pain with urination
-
Chest pain, shortness of breath, or cough that won’t go away
-
Upset stomach (nausea) and vomiting
-
Dizziness or fainting
-
Leg swelling or pain
Follow-up
Recovery time will vary for each person. It may take as long as 4 to 6 weeks. You will need to see your provider for follow-up. This is to remove any stitches or staples and to check your healing progress.
Risks and possible complications
These vary depending on the reason for the surgery. The most common risks and possible complications include:
-
Bleeding
-
Infection
-
Can't find the cause of the problem, so more surgery or other treatments may be needed
-
Incision doesn't heal well
-
Damage, injury, or problems with the bowels
-
Risks of reaction to anesthesia
Online Medical Reviewer:
Jen Lehrer MD
Online Medical Reviewer:
Raymond Kent Turley BSN MSN RN
Online Medical Reviewer:
Rita Sather RN
Date Last Reviewed:
2/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.