Laparoscopic Varicocelectomy
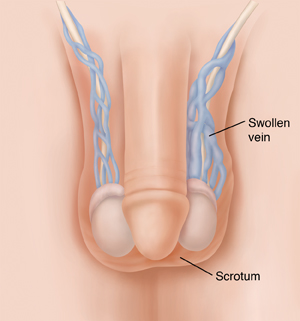
Varicocelectomy is surgery to fix a varicocele. A varicocele is swelling of veins in the scrotum. This swelling is due to blood backing up in the veins. A varicocele can cause pain or a heavy feeling in the scrotum but is often painless. It can also cause problems with fertility. During the surgery, the swollen veins are cut, and the ends are closed off. Other veins in the groin area then take over carrying the blood supply. The surgery may be done with a method called laparoscopy or through open surgery. During laparoscopy, a thin, lighted tube or scope (called a laparoscope) is used. The scope allows the healthcare provider to work through a few small cuts (incisions).
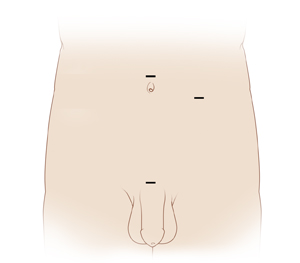 |
| Possible incision sites |
Getting ready for surgery
Get ready for the surgery as you’ve been told. In addition:
-
Tell your healthcare provider about all the medicines you take. This includes prescription medicines and over-the-counter medicines, vitamins, herbs, and other supplements. It also includes any blood thinners, such as warfarin, clopidogrel, or daily aspirin. You may need to stop taking some or all of them before surgery.
-
Follow any directions you are given for not eating or drinking before surgery. This includes coffee, water, gum, and mints. (If you have been instructed to take medicines, take them with a small sip of water.)
The day of surgery
This surgery takes 1 to 2 hours. You’ll likely go home the same day.
Before the surgery begins
-
An IV (intravenous) line is put into a vein in your arm or hand. This supplies fluids and medicine (such as antibiotics).
-
You may be given a medicine to prevent blood clots.
-
To keep you pain-free during the surgery, you’re given general anesthesia. This medicine puts you into a deep sleep-like state during the surgery. A tube may be inserted into your throat to help you breathe.
-
A thin tube (catheter) is placed in your bladder to drain urine.
During the surgery
-
The healthcare provider makes a few small incisions in the belly (abdomen).
-
The scope is placed through one of the incisions. It sends live pictures of the inside of the abdomen to a video screen.
-
The abdomen is filled with gas. This makes space for the healthcare provider to see and work.
-
Using tools placed through the other incisions, the swollen veins are cut. The ends may be sealed with tiny clips. Or the ends may be cauterized, which means heat may be used to seal them.
-
When the surgery is done, all tools are removed. The incisions are closed with stitches or staples.
The healthcare provider will begin with laparoscopy. But they may need to change to open surgery for safety reasons. Open surgery is done using an incision in the abdomen or the groin. You’ll be told more about this possibility before surgery.
After the surgery
You’ll be taken to a recovery room to rest until the anesthesia wears off. You may feel sleepy and nauseated. If a breathing tube was used, your throat might be sore at first. You’ll be given medicines to manage any pain. The catheter will be removed from your bladder. When you’re ready to go home, you’ll be released to an adult family member or friend.
Recovering at home
Have someone help you at home as your healing begins. Follow all the instructions you’ve been given. Make sure to:
-
Take all medicines as directed.
-
Care for your incisions as instructed.
-
Apply ice or a cold compress to the scrotum for 10 minutes at a time for the first 48 hours. This helps reduce swelling. To make an ice pack, put ice cubes in a plastic bag that seals at the top. Wrap the bag in a clean, thin towel or cloth. Never put ice or an ice pack directly on the skin.
-
Follow your healthcare provider’s guidelines for showering. Don't swim, take a bath, use a hot tub, or do other activities that cause the incision to be covered with water until your provider says it’s OK.
-
Not have sex for 1 to 2 weeks.
-
Not do any heavy lifting and other strenuous activities, as directed.
-
Not drive until your provider says it’s OK. Don’t drive if you’re taking medicines that make you drowsy or sleepy.
-
Not strain to pass stool. If needed, take stool softeners as directed by your provider.
Call 911
Call 911 if you have:
-
Chest pain
-
Trouble breathing
When to call your healthcare provider
Call your healthcare provider right away if you have any of the following:
-
Fever of 100.4° F ( 38°C ) or higher, or as directed by your healthcare provider
-
Symptoms of infection at an incision site, such as more redness or swelling, warmth, pain that gets worse, or bad-smelling drainage
-
Pain that can't be controlled with medicines
-
Swelling in the scrotum that doesn’t go away
-
Trouble passing urine
-
Nausea or vomiting that won’t go away
-
Pain or swelling in the legs
Follow-up care
You’ll have follow-up visits so your healthcare provider can check how well you’re healing. If your stitches or staples need to be removed, this will likely be done in 7 days. If you’re concerned about your fertility, a sample of your semen can be checked in about 3 to 4 months. This helps see if the number and quality of your sperm have improved.
Risks and possible complications
Possible risks of this procedure include:
-
Infection
-
Bleeding, blood clots
-
Return of the varicocele
-
Failure to restore fertility
-
Fluid around a testicle (hydrocele)
-
Shrinking (atrophy) of a testicle
-
Damage to nearby nerves, blood vessels, or organs (including the intestine)
-
Short-term (temporary) decrease in sperm count
-
Long-term (chronic) pain
-
Risks of anesthesia. The anesthesiologist or nurse anesthetist will discuss these with you.
Online Medical Reviewer:
Marc Greenstein MD
Online Medical Reviewer:
Raymond Kent Turley BSN MSN RN
Online Medical Reviewer:
Tennille Dozier RN BSN RDMS
Date Last Reviewed:
3/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.