Rotator Cuff Repair
What is a rotator cuff repair?
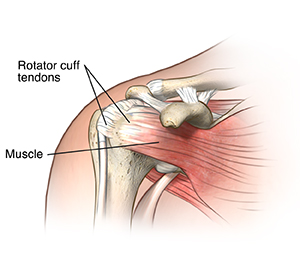
The rotator cuff is made up of muscles and tendons that hold the shoulder in place. It’s one of the most important parts of the shoulder. It allows you to lift your arm and reach up. An injury to the rotator cuff, such as a tear, may happen suddenly when falling on an outstretched hand or develop over time due to repetitive activities. Rotator cuff degeneration and tears may also be caused by aging.
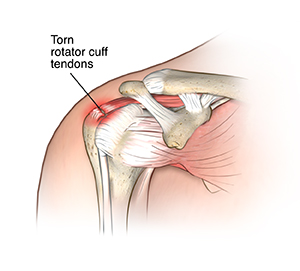
If your rotator cuff is injured, it may need surgery to repair it. This may include shaving off bone spurs that are pinching the shoulder or repairing torn tendons or muscles in the shoulder. This usually involves reattaching the tendon to the head of the humerus. Surgical techniques that may be used to repair a tear of the rotator cuff include arthroscopy, open surgery, or a combination of both. The goal of rotator cuff repair surgery is to help restore the function and flexibility of the shoulder and to relieve the pain that can’t be controlled by other treatments.
Why might I need a rotator cuff repair?
Shoulder injuries are common. Athletes and construction workers often have rotator cuff injuries from repetitive movement and overuse of the shoulder. The rotator cuff may be damaged from a fall or other injury to the shoulder. Damage may also happen slowly over time. The damage may be from:
-
Strains or tears in the rotator cuff
-
Inflammation of the bursa (bursitis) in the shoulder
-
Inflammation of the tendons (tendinitis) in the shoulder
Recurrent pain, limited ability to move the arm, and muscle weakness are the most common symptoms.
If medical treatments aren't working, rotator cuff repair surgery may be a treatment that helps. Medical treatments for rotator cuff injury may include:
Rotator cuff surgery may be done using an arthroscope. An arthroscope is a small, tube-shaped tool that is inserted into a joint. It is made of a system of lenses, a small video camera, and a light for viewing. The camera is connected to a video monitoring system that lets the surgeon view a joint through a very small incision. The arthroscope is often used along with other tools that are put through another small incision.
An open repair may be done if the rotator cuff injury can’t be repaired using arthroscopy. In some cases, a tendon graft or joint replacement may be needed.
There may be other reasons for your healthcare provider to recommend rotator cuff repair.
What are the risks of a rotator cuff repair?
As with any surgical procedure, complications can happen. Some possible complications may include:
The joint pain and weakness may not be relieved by the surgery. You may not recover full range of motion in the shoulder joint.
Nerves or blood vessels in the area of surgery may be injured. This results in weakness or numbness.
There may be other risks depending on your specific medical condition. Tell your provider about any concerns you have before the procedure.
How do I get ready for a rotator cuff repair?
-
Your provider will explain the procedure to you. You can ask questions.
-
You'll be asked to sign a consent form that gives your permission to do the procedure. Read the form carefully and ask questions if something isn't clear.
-
In addition to a complete medical history, your provider may do a complete physical exam to make sure that you're in good health before undergoing the procedure. You may undergo blood tests or other diagnostic tests.
-
Tell your provider if you're sensitive to or allergic to any medicines, latex, tape, and anesthetic agents (local and general).
-
Tell your provider about all prescription and over-the-counter medicines you take. Also tell them about any vitamins and herbal supplements you're taking.
-
Tell your provider if you have a history of bleeding disorders or if you're taking any blood-thinning (anticoagulant) medicines, aspirin, or other medicines that affect blood clotting. You may need to stop taking these medicines before the procedure.
-
If you're pregnant or think that you could be pregnant, tell your provider.
-
Follow all directions you're given about not eating or drinking before your procedure.
-
You may get a medicine (sedative) before the procedure to help you relax. Arrange for a trusted adult to drive you home after surgery.
-
You may meet with a physical therapist before your surgery to talk about rehabilitation.
-
Based on your medical condition, your provider may request other specific preparation.
What happens during a rotator cuff repair?
Rotator cuff repair may be done on an outpatient basis or as part of your stay in a hospital. Procedures may vary depending on your condition and your provider’s practices.
Rotator cuff repair may be done while you're asleep under general anesthesia or while you're awake under local or regional anesthesia. If regional anesthesia is used, you'll have no feeling in your shoulder. The type of anesthesia will depend on the specific procedure being done. Your provider will discuss this with you in advance.
Generally, rotator cuff repair surgery follows this process:
-
You'll be asked to remove clothing and given a gown to wear.
-
An IV (intravenous) line may be started in your arm or hand.
-
You'll be positioned on the operating table.
-
The anesthesiologist or nurse anesthetist will continuously monitor your heart rate, blood pressure, breathing, and blood oxygen level during the surgery.
-
The skin over your surgical site will be cleaned with an antiseptic solution.
-
Your surgeon will make a cut (incision) in the shoulder area. The incision will vary depending on the type of surgery (open surgery, arthroscopy, or a combination of both) that may be done.
-
The arthroscope (if used) will be put through the incision.
-
Other incisions may be made to use other small grasping, probing, or cutting tools.
-
The surgeon may fix or replace injured tendons and muscles with a graft tendon.
-
Bone spurs will be removed if there are any.
-
The incision will be closed with stitches or surgical staples.
-
A sterile bandage or dressing will be applied.
What happens after a rotator cuff repair?
After surgery you'll be taken to the recovery room for close monitoring as you wake up from anesthesia. . Your recovery process will vary depending on the type of anesthesia that is given and the type of surgery that’s done. The circulation and sensation of your arm will be monitored. Once your blood pressure, pulse, and breathing are stable and you're alert, you'll be taken to your hospital room or discharged to your home.
You may be given an immobilizer or sling before you go home.
Once you’re home, it’s important to keep the surgical area clean and dry. Your surgeon will give you specific bathing instructions. The stitches or surgical staples will be removed during a follow-up office visit.
Take a pain reliever for soreness as recommended by your healthcare provider. Aspirin or certain other pain medicines may increase the chance of bleeding. Be sure to take only recommended medicines.
To help reduce swelling, you may be asked to apply an ice bag to the shoulder several times per day for the first few days. You should keep the sling or immobilizer on as directed by your provider.
Your provider will arrange for an exercise rehabilitation program to help you regain muscle strength, flexibility, and function of your shoulder. Expect full recovery to take up to 4 to 6 months.
Call your healthcare provider right away if you have any of these symptoms:
-
Fever or chills
-
Redness, swelling, bleeding, or other drainage from the incision site
-
Increased pain around the incision site
-
Numbness or tingling in the affected arm or hand
You may resume your normal diet unless your provider advises you differently.
You shouldn't drive until your surgeon tells you to. Other activity restrictions may apply. Full recovery from the surgery may take several months.
Your surgeon may give you other instructions after the procedure, depending on your particular situation.
Next steps
Before you agree to the test or the procedure make sure you know:
-
The name of the test or procedure
-
The reason you're having the test or procedure
-
What results to expect and what they mean
-
The risks and benefits of the test or procedure
-
What the possible side effects or complications are
-
When and where you're to have the test or procedure
-
Who will do the test or procedure and what that person’s qualifications are
-
What would happen if you didn't have the test or procedure
-
Any alternative tests or procedures to think about
-
When and how you'll get the results
-
Who to call after the test or procedure if you have questions or problems
-
How much you'll have to pay for the test or procedure